Today, we dive into the often underestimated and overlooked powerhouse of the body—the glute muscles. Yes, those muscles that are the real MVPs in shaping and supporting our bottoms.
How many times have you heard a fitness instructor or physiotherapist say “use your glutes” or “you know what your problem is… you just don’t use your glutes”. But when does someone actually show you where your glutes are, how to activate them, and what they do?
Sometimes we forget that the simplest knowledge can be the most powerful, so today we are breaking it down. Grab your water bottle, put on your favourite workout playlist, and let's talk glutes!
Location, Location, Location: Where Are Your Glutes?
First things first, where exactly are these glutes we're talking about? Well, they're the group of muscles in your buttocks, made up of three individual muscles: the gluteus maximus, gluteus medius, and gluteus minimus.
Gluteus Maximus: The Powerhouse of Extension
This is the biggest of the three glute muscles and also the most powerful. It is the one that sits right on the surface and can give you the J.Lo definition. Beyond having a cute peach it is also the prime mover in hip extension. Meaning when you lift your leg back behind you, your gluteus maximus is the main driver of that movement. It is important in so many daily movements, but recently with a rise in desk jobs, a lot of us don’t use this main muscle as often as we should, causing it to atrophy (or shrink).
Gluteus Medius: The Underrated Middle Sister
Gluteus medius never receives the attention it should. It is the prime mover of hip abduction (lifting your leg to the side) and a big contributor to hip extension and rotation, as well as hip stability. A weak gluteus medius or poor activation can lead to a host of issues like back pain, IT Band syndrome, and poor hip and knee mechanics when running, walking, and squatting. When someone has a weak gluteus medius we often see a hip tilt on a single leg called a Trendelenburg sign.
This little gal needs to be worked often and in most physiotherapist opinions everyone should have an isolated hip abduction exercise in their physical fitness routine. You want to keep the gluteus medius strong and healthy.
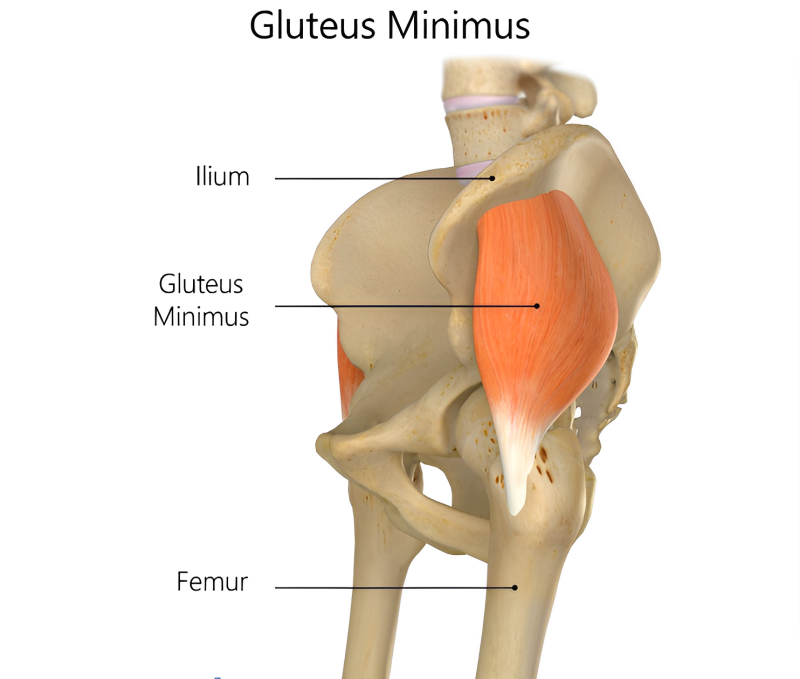
Gluteus Minimus: The Happy Helper
Gluteus Minimus is the smallest of the glute group, and its primary job is to help with hip stability and hip abduction. Single-leg exercises tend to target this muscle group the most and it is happy to tag along when working out the two bigger muscles in its group.
Getting to Know Your Glutes: What Do They Do?
We touched on this a little bit above, but in a more general sense the glutes are more than just a cushy seat for your favourite chair—they're involved in a range of movements, from standing up straight, to walking, running, and even maintaining balance. Strong glutes help support your lower back, improve posture, and maintain proper hip and knee mechanics. In short, they're the unsung heroes of your body!
Activating the Power: How to Use Your Glutes
It’s time to put those glutes to work! The key to activating your glutes is to focus on engaging them during exercises, creating a stronger mind-body connection. If you aren’t used to using your glutes you may have to consciously think about it at the start. Try squeezing your glutes in a chair just to locate them first and then transfer that standing or at the top of a squat. These simple actions can help strengthen and tone these muscles over time and help create a strong connection.
Glute Exercises to Get Started:
Now, the fun part—let's explore some exercises that will fire up the glutes:
Squats:
Stand with your feet shoulder-width apart.
Lower your body as if you're sitting back into a chair, keeping your chest up and knees behind your toes.
Squeeze your glutes as you return to the starting position.
Reverse Lunges:
Take a step backwards with one foot, lowering your body until both knees are bent at a 90-degree angle.
Push off the back foot, engaging your glutes, and return to the starting position.
Repeat on the other leg.
Glute Bridges:
Lie on your back with your knees bent and feet flat on the floor.
Lift your hips toward the ceiling, squeezing your glutes at the top.
Lower your hips back down and repeat.
Monster Walks:
Start a band around the arches of your feet or ankles.
Take small steps in a lateral direction, keeping tension on the band
Try 10 steps to the left and 10 steps to the right.
Resisted Hip Abduction
Stand on a single leg with a band around your ankles
Lift your non-standing leg out to the side, inline with your standing leg
Lower the leg back to the starting position and repeat
Single Leg Deadlifts
Standing on a single leg, hinge forward at your hip
Lift the back leg at the same rate as you tilt forward
Return to an upright position by squeezing your glutes
Keep the sets and reps of all exercises simple, begin with 3 sets x 10 reps (on each side - if the exercise is on a single leg), and progress to 12-15 reps once you are able.
Incorporate some or all of these exercises into your routine, and your glutes will thank you later. Remember, consistency is key, so make sure to gradually increase intensity and challenge yourself as you progress.
If you want something more individualized or would like someone to show you technique and walk you through the paces, book an appointment with one of our clinicians. You can do this by phone at 250-723-5112, or online at https://www.portalberniphysiotherapy.ca