Tendon pain is one of the most common musculoskeletal issues seen in both active and sedentary populations. Whether it shows up as Achilles pain, tennis elbow, patellar tendon pain, or rotator cuff irritation, these injuries are notoriously slow to resolve. For decades, the standard advice was simple: rest, ice, and avoid anything that aggravates symptoms. While these strategies can be useful early on to calm pain, we now understand that rest alone does not lead to optimal tendon healing. In many cases, it may actually delay recovery.
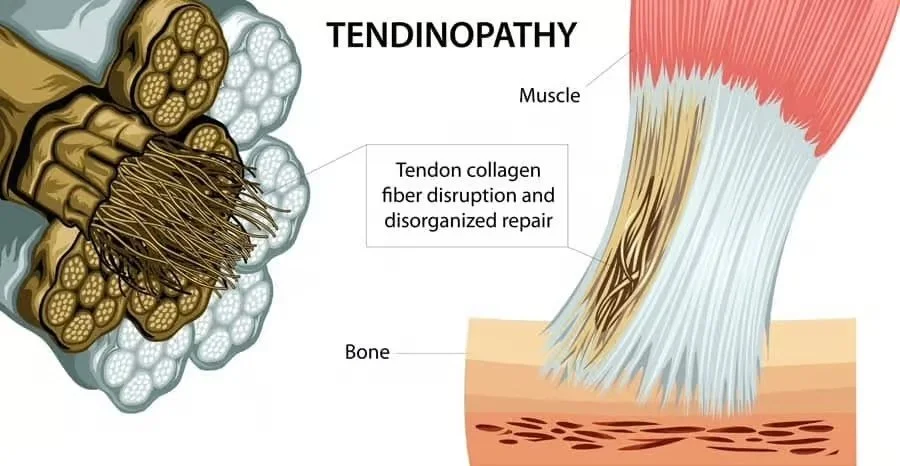
Tendons connect muscle to bone and are designed to tolerate high levels of load. Unlike muscle, however, they have a relatively limited blood supply, which is one reason they heal more slowly. When a tendon becomes irritated or injured, the collagen fibers that give it strength and structure become disrupted. If the tendon is not appropriately stressed during the healing process, the body may lay down new collagen in a disorganized, weaker pattern. This can result in lingering pain, reduced strength, and a tendon that is poorly prepared for return to activity. This is why so many people experience recurring flare-ups after a period of rest—symptoms may settle, but the underlying tissue has not been properly reconditioned.
Ice and rest still have a place in the very early stages of tendon injury, particularly when pain is intense and movement is significantly limited. However, relying on them as the primary long-term strategy can be problematic. By avoiding load altogether, the tendon is deprived of the very stimulus it needs to rebuild. As a result, stiffness increases, load tolerance decreases, and return to sport or daily activity often leads to reinjury.
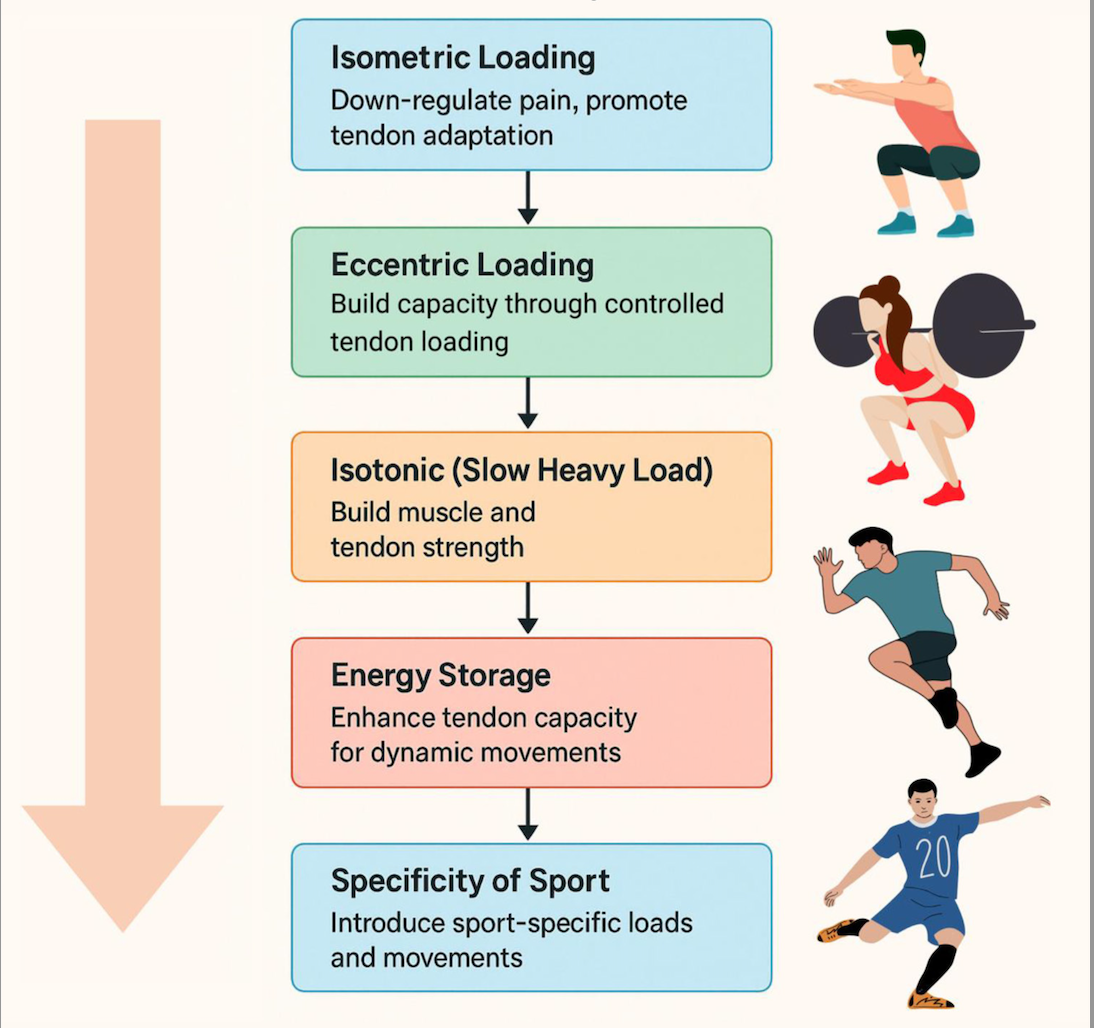
Current research now strongly supports progressive mechanical loading as the cornerstone of effective tendon rehabilitation. One of the most valuable early-stage tools is isometric exercise, which involves contracting a muscle without visible joint movement. These types of exercises place controlled stress through the tendon without excessive strain. Research has shown that isometric loading can help stimulate collagen production, encourage proper realignment of tendon fibers, and significantly reduce pain. A commonly used protocol involves 30-second holds, repeated four to five times, performed once or twice per day, depending on the individual, the joint effected and the severity of the condition being treated. This approach allows the tendon to begin adapting safely before advancing to more dynamic movement.
As symptoms improve, tendon loading must also progress. Tendons adapt to the demands placed on them, meaning rehabilitation must gradually expose the tissue to higher loads through slow strengthening exercises and eventually to faster, more powerful movements. This staged approach is what allows the tendon to regain its ability to tolerate real-world forces such as walking, running, jumping, lifting, and sport-specific movements. Skipping these stages or returning to full activity too quickly is one of the most common reasons tendon injuries become chronic.
Nutrition may also play a supportive role in tendon recovery. Emerging research suggests that taking hydrolyzed collagen along with vitamin C prior to tendon-loading exercise may help improve collagen synthesis. Vitamin C is essential for collagen formation, and when paired with targeted loading, this strategy may assist the body in building healthier tendon tissue. While supplementation alone will not heal a tendon, it may be a useful adjunct when combined with a structured rehabilitation program.
It is also important to recognize that not all tendon injuries should be treated the same way. The angle of loading, joint position, and type of exercise must be carefully selected based on the location of the injury. For example, the rehabilitation demands of tennis elbow differ significantly from those of Achilles or patellar tendon pain. What is considered appropriate load for one tendon may be excessive or ineffective for another. This is why individualized physiotherapy assessment and programming are critical for safe and effective recovery.
True tendon rehabilitation is rarely a quick fix. Instead, it follows a progressive process that typically includes early pain management, controlled loading through isometrics, gradual strengthening with slow and heavy resistance, and eventually higher-level energy storage and release activities such as hopping, running, or sport-specific training. Each phase builds on the one before it, ensuring the tendon is prepared for the demands that will be placed on it long term.
The key takeaway is this: tendons need stress to heal. While rest and ice can provide short-term symptom relief, they do not rebuild the strength, structure, and resilience required for lasting recovery. Appropriate exercise is not something to fear in tendon rehab—it is the very tool that drives healing. When guided correctly, progressive loading helps restore function, reduce pain, and prevent future flare-ups.
If you are dealing with persistent tendon pain that keeps returning despite rest, it may be a sign that the tissue has not been properly reconditioned for the demands of your work, sport, or daily life. A structured, individualized tendon-loading program guided by a physiotherapist can make the difference between ongoing frustration and a confident return to movement.